Cancer - Overview
Advances in medical science have improved outcomes for many cancer patients, but the fight against cancer continues as scientists, healthcare professionals, and organizations work tirelessly to understand the disease and develop innovative therapies to combat it. However, there is encouraging news that the treatment options for cancer are now easily accessible and continually advancing.
Cancer treatment is a comprehensive approach aimed at controlling, managing, or eliminating cancer cells from the body. The choice of treatment depends on various factors, including the type and stage of cancer, overall health condition of the patient, and individual preferences. There are several main treatment modalities used in cancer treatment, often used in combination:
Surgery: Surgical intervention involves the removal of tumors and surrounding tissues. It is typically used for solid tumors and can be curative if the cancer has not spread to other parts of the body.
Chemotherapy: Chemotherapy involves the use of powerful drugs to kill cancer cells or prevent their growth. It is often administered systemically, targeting cancer cells throughout the body. Chemotherapy can be used as a primary treatment, in combination with surgery or radiation, or as palliative care to alleviate symptoms.
Radiation therapy: Radiation therapy uses high-energy X-rays or other forms of radiation to destroy cancer cells or shrink tumors. It can be delivered externally (external beam radiation) or internally (brachytherapy) and is often combined with other treatments.
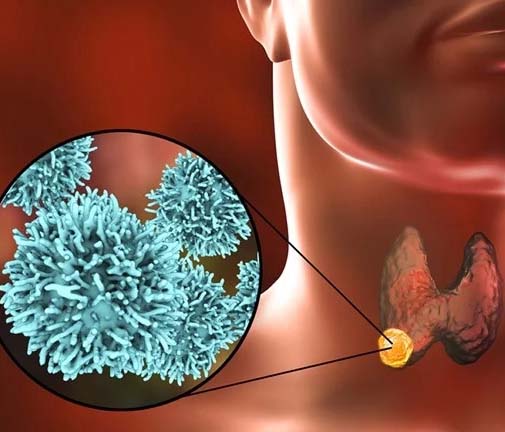
Immunotherapy: Immunotherapy harnesses the body’s immune system to recognize and attack cancer cells. It can be done through the use of immune checkpoint inhibitors, monoclonal antibodies, cancer vaccines, or adoptive cell therapy. Immunotherapy has shown promising results in certain types of cancer, helping to stimulate the immune response against cancer cells.
Targeted therapy: Targeted therapy uses drugs or other substances to target specific molecules or pathways involved in the growth and spread of cancer cells. It aims to block the signals that support cancer cell growth, leading to more targeted and precise treatment.
Hormone therapy: Hormone therapy is used to treat hormone-sensitive cancers such as breast and prostate cancer. It involves the use of medications that interfere with the production or action of certain hormones, which can help slow down or stop the growth of cancer cells.
Stem cell transplant: Stem cell transplant, also known as a bone marrow transplant, involves replacing damaged or destroyed bone marrow with healthy stem cells to promote the growth of new, healthy cells. It is commonly used in the treatment of certain blood cancers and other conditions.
It is important to note that cancer treatment plans are personalized and may vary from patient to patient. Multidisciplinary teams consisting of oncologists, surgeons, radiation oncologists, and other healthcare professionals collaborate to determine the most appropriate treatment approach for each individual. Moreover, supportive care, including pain management, psychological support, and lifestyle modifications, is an integral part of cancer treatment to improve the overall well-being of patients.
Advancements in cancer research have led to the development of new treatment options, targeted therapies, and improved outcomes for many cancer patients. However, it is essential to emphasize the importance of early detection, regular screenings, and adopting a healthy lifestyle to reduce the risk of developing cancer. Ongoing research and clinical trials continue to expand our understanding of cancer and contribute to the development of more effective and personalized treatment strategies.
Cancer - Symptoms
Cancer treatment can often lead to various symptoms and side effects that can impact a person’s well-being during their journey. These symptoms can vary widely depending on the type of cancer, stage of cancer, and the specific treatment being administered. Common symptoms experienced during cancer treatment include fatigue, nausea and vomiting, loss of appetite, hair loss, pain, changes in bowel or bladder function, skin changes, cognitive changes, and emotional distress. It’s important for individuals undergoing cancer treatment to communicate these symptoms to their healthcare team, as they can provide supportive care and interventions to help manage and alleviate these symptoms, improving the overall quality of life during treatment.
It’s crucial to remember that symptom management is a key aspect of cancer treatment, and healthcare providers work closely with patients to minimize the impact of these symptoms. They may prescribe medications to alleviate nausea and pain, recommend dietary adjustments to address appetite changes, provide resources for managing hair loss, offer strategies for coping with cognitive changes, and provide emotional support throughout the treatment process. Open and honest communication with the healthcare team is essential to ensure that symptoms are addressed promptly and effectively, enabling individuals to better tolerate and manage their cancer treatment.
Cancer - Pre-Procedure
Before undergoing cancer treatment, there are several important pre-procedure steps that need to be taken to ensure the best possible outcomes. The first step is a comprehensive evaluation by the healthcare team, which may include oncologists, surgeons, radiologists, and other specialists. This evaluation involves a thorough medical history review, physical examination, and diagnostic tests to determine the type and stage of cancer. These assessments help guide treatment decisions and determine the most appropriate treatment plan for the individual.
Once the treatment plan is established, pre-procedure preparations may include various steps such as obtaining informed consent, discussing potential risks and benefits, and addressing any concerns or questions the patient may have. In some cases, additional tests or procedures may be required to gather more specific information about the cancer or to assess the patient’s overall health and suitability for the treatment.
Preparations may also involve lifestyle adjustments, such as quitting smoking, managing chronic health conditions, or making dietary modifications to optimize the body’s readiness for treatment. This pre-procedure phase plays a crucial role in ensuring that the individual is mentally and physically prepared for their cancer treatment and that the necessary precautions and considerations are taken to maximize treatment effectiveness and minimize potential risks.
Cancer - During Procedure
Chemotherapy: Chemotherapy involves the administration of powerful medications that target and kill cancer cells. The drugs may be given orally, intravenously, or through other methods. During chemotherapy sessions, patients may receive treatment in an outpatient setting or as an inpatient, depending on the specific treatment regimen. Healthcare professionals closely monitor the patient’s vital signs and administer the medications according to a prescribed schedule. Throughout the procedure, the patient’s comfort and well-being are a priority, and any potential side effects or adverse reactions are closely monitored and managed.
Radiation therapy: Radiation therapy uses high-energy beams to target and destroy cancer cells. The procedure is typically administered in a specialized radiation therapy department. Before the treatment session, the patient will be positioned carefully on the treatment table, and imaging techniques may be used to ensure accurate targeting of the radiation beams. The radiation therapist will leave the room during the actual treatment, but the patient will be monitored through audio and video systems. Multiple treatment sessions may be required over a designated period, and the healthcare team closely monitors the patient’s response to treatment, adjusting the dosage and approach as needed.
Surgery: Surgical procedures for cancer treatment involve the removal of tumors or affected tissues. The surgical approach and extent of the procedure will depend on factors such as the type, size, and location of the tumor. Surgeons perform the surgery in an operating room under general or local anesthesia. Throughout the procedure, an anesthesiologist closely monitors the patient’s vital signs and ensures their comfort. The surgical team takes precautions to minimize the risk of complications and to ensure the best possible outcome. After the surgery, the patient is closely monitored during the recovery period, and appropriate pain management and post-operative care measures are implemented.
Cancer - Post-Procedure
After undergoing cancer treatment, the post-procedure phase is crucial for monitoring and supporting the patient’s recovery and overall well-being. Depending on the type of treatment received, the post-procedure period may involve different aspects of care. Patients may experience a range of physical and emotional changes during this time, and the healthcare team plays a vital role in providing necessary support and follow-up care. They closely monitor the patient’s condition, assess treatment response, manage any side effects or complications, and adjust the treatment plan as needed.
Additionally, patients may receive guidance on managing symptoms, pain management, wound care, and dietary or lifestyle modifications to aid in the healing process. Emotional support, counseling, and access to support groups may also be provided to address the psychological impact of cancer treatment. The post-procedure phase is a critical time for ongoing care and support, with the goal of ensuring optimal recovery and promoting the patient’s overall well-being.
Cancer - Risk & Complications
The risk and complications associated with cancer can vary from case to case. Each individual may respond differently to their respective treatment.
Short-term side effects: Short-term side effects typically refer to temporary symptoms experienced during and immediately after the treatment.
Long-term side effects: On the other hand, long-term side effects can persist for a month, several years, or even throughout a person’s lifetime.
Cancer - Doctors
Cancer - Hospitals
Request a CallBack